Unicompartmental Knee replacement
One of the other main types of joint replacement procedure I perform is Unicompartmental Knee Replacement. This factsheet is for people who are planning to have a Unicompartmental Knee Replacement procedure. Unicompartmental Knee Replacement means replacing one part of a knee joint that has been damaged or worn away.
Your knee joint is made up by the ends of your thigh bone (femur) and shin bone (tibia). These bones normally glide over each other easily because they are covered by smooth cartilage. If your cartilage is damaged by injury or worn away by arthritis for example, it can make your joint painful and stiff. A new knee joint usually improves mobility and reduces pain, although your new knee will not be able to bend quite as far as a normal knee joint. It is important to realize that your new knee is an artificial, mechanical joint and will not feel quite the same as your own knee did before it developed pain.
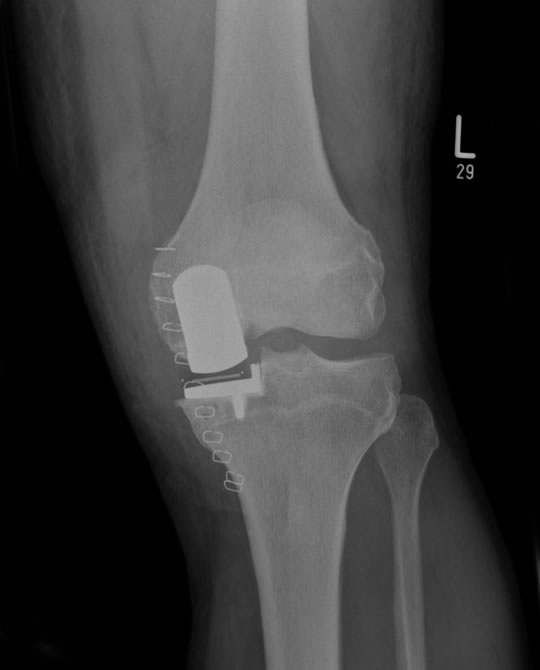
By being listed for a Unicompartmental Knee replacement, Mr Clifton has decided your main area of arthritis is restricted to the inside (medial side) of your knee. You may also have some arthritis under the knee cap which is relatively asymptomatic. You will NOT have any severe arthritis over the outside (lateral side) of your knee. The mechanical parts are usually made of metal such as cobalt chrome alloy or titanium and plastic (polyethylene). A good Unicompartmental knee replacement will last up to 20 years with the vast majority lasting longer than 10 years or more (Figure 1).
Figure 1 Patient with a new Unicompartmental Knee Replacement performed by Mr Clifton
Surgery is usually recommended only if non-surgical treatments, such as physiotherapy and exercise, taking medicines or using physical aids like a walking stick, no longer help to reduce pain or improve mobility.
The operation usually requires a hospital stay of about three days and it's done under general or spinal anaesthesia. General aneasthesia means you will be asleep during the operation. Spinal anaesthesia completely blocks feeling from your waist down and you will stay awake during the operation. If you're having a general anaesthetic, you will be asked to follow fasting instructions. This means not eating or drinking, typically for about six hours before a general anaesthetic. However, it's important to follow your anaesthetist's advice. Before your operation at the hospital, a nurse will check your heart rate and blood pressure, and test your urine.
Mr Clifton will discuss with you what will happen before, during and after your procedure, and any pain you might have. This is your opportunity to understand what will happen, and you can help yourself by preparing questions to ask about the risks, benefits and any alternatives to the procedure. This will help you to be informed, so you can give your consent for the procedure to go ahead, which you will be asked to do by signing a consent form.
You may be asked to wear a compression stocking on the unaffected leg to help prevent blood clots forming in your veins (deep vein thrombosis, DVT). You may need to have an injection of an anticlotting medicine called heparin as well as, or instead of stockings.
A Unicompartmental knee replacement usually takes up to two hours depending on the complexity of the deformity and bone loss. Mr Clifton will make a single cut (10 cm long) down the front of your knee. Worn and damaged surfaces are removed from both the end of your thigh bone and the top of your shin bone. To preserve side to side stability, we don't remove your collateral ligaments. Mr Clifton will shape the surfaces of your thigh and shin bones to fit the artificial knee joint and then fit the new joint over both bones fixing it with Bone Cement. After your new joint has been fixed, Mr Clifton will close your wound with stitches or clips and cover with a dressing. Your knee will be tightly bandaged to help minimize swelling.
You will need to rest until the effects of the anaesthetic have passed. You may not be able to feel or move your legs for several hours after an epidural anaesthetic. You may need pain relief to help with any discomfort as the anaesthetic wears off. For the first day or so, you may have an intermittent compression pump attached to special pads on your lower legs. By inflating the pads, the pump encourages healthy blood flow and helps to prevent DVT. You may also have a compression stocking on your unaffected leg. This helps to maintain circulation. A physiotherapist (a specialist in movement and mobility) will usually guide you daily through exercises to help your recovery. You will be in hospital until you can walk safely with the aid of sticks or crutches. When you're ready to go home, you will need to arrange for someone to drive you. Your nurse will give you some advice about caring for your knee and a date for a follow-up appointment before you go home. The length of time your dissolvable stitches will take to disappear depends on what type you have. However, for this procedure they should usually disappear in about six weeks. Non-dissolvable stitches and clips are removed 10 to 14 days after surgery.
If you need them, you can take over-the-counter painkillers such as paracetamol or ibuprofen. Follow the instructions in the patient information leaflet that comes with the medicine and ask your pharmacist for advice. The physiotherapy exercises are a crucial part of your recovery, so it's essential that you continue to do them for at least two months. You will be able to move around your home and manage stairs. You will find some routine daily activities, such as shopping, difficult for a few weeks. You may need to use a walking stick or crutches for up to six weeks. You may be asked to wear compression stockings for several weeks at home. When you're resting, raise your leg and support your knee to help prevent swelling in your leg and ankle. Depending on the type of work you do, you can usually return to work after six to 12 weeks. Follow Mr Clifton's advice about driving. You shouldn't drive until you are confident that you could perform an emergency stop without discomfort.
Unicompartmental knee replacement surgery is commonly performed and generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications of this procedure.
These are the unwanted, but mostly temporary effects of a successful treatment, for example feeling sick as a result of the general anaesthetic. Your knee will feel sore and may be swollen for up to six months. You will have a scar over the front of the knee. You may not have any feeling in the skin around your scar. This can be permanent, but should improve over two years.
This is when problems occur during or after the operation. Most people are not affected. The possible complications of any operation include an unexpected reaction to the anaesthetic, excessive bleeding or developing a blood clot, usually in a vein in the leg (DVT).
Specific complications of knee replacement are uncommon, but can include those listed below.
- Infection of the wound or joint. Antibiotics are given during and after surgery to help prevent this.
- Unstable joint. Your knee joint may become loose and you may require further surgery to correct this.
- Damage to nerves or blood vessels. This is usually mild and temporary.
- Scar tissue. This can build up and restrict your movement. Further surgery may be needed to correct this.
The artificial knee joint usually lasts for up to 20 years, after which you may need to have it replaced. More often than not this is with a Primary Total Knee Replacement (Figure 2).
Figure 2